Q and A on ‘gold standard’ stem cells
British scientists have achieved the ‘holy grail’ and created a gold standard stem cell line. But why is this something to get excited about? Channel 4 News answers your questions.
Why are stem cells in the news this week?
After 10 years of research, scientists from King’s College London have created the first clinical grade human embryonic stem cell (ESC) lines and donated them to the UK Stem Cell Bank
What is different about these ‘gold standard’ stem cell lines?
This batch of ESCs are, for the first time, free from animal-derived products. They have been grown directly from embryos and are ‘xeno-free’ stem cells.
Why does this matter?
Stem cells that use animal reagents to stimulate growth can be used for research, but can only be upgraded for clinical use after extensive testing and at a high risk, which takes time and significant expense.
The new cells are already at the regulatory clinical standards, so they take scientists one-step closer to using stem cells in therapeutic medicine and have the potential to become the ‘gold standard’ line for developing medical treatment.
We had to get to the point where everything we’re using is animal free, or in some way has been tested to be safe or its provenance known – you can’t have something that has been exposed to pig, mouse or cow injected into humans. Peter Braude, King’s College London
Why are the new ESCs better than cells from animal-derived products?
‘Research grade’ stem cells are derived in the presence of animal products and are subject to a huge amount of testing to assess how they would react before being upgraded to ‘clinical’ and then used in trials.
With the new xeno-free cells, researchers are starting with ‘clean’ cells, Professor Peter Braude, Emeritus Professor of Obstetrics and Gynaecology at King’s, told Channel 4 News.
“We had to get to the point where everything we’re using is animal free, or in some way has been tested to be safe or its provenance known – you can’t have something that has been exposed to pig, mouse or cow injected into humans,” said Professor Braude.
“The ‘holy grail’ is where you start the line from the point where it is clean enough to be used for clinical therapy – all the ingredients are clean.”
How are ESCs grown?
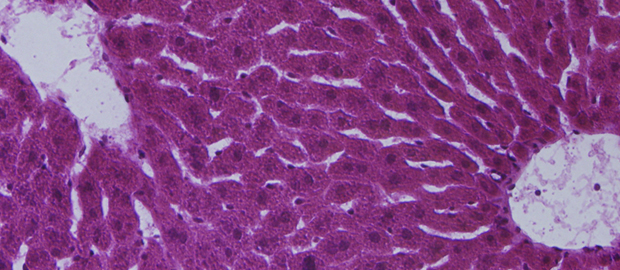
Embryonic stem cells are grown in a laboratory and retain their capacity to develop into specialised cell types, such as nerve or heart muscle cells, which can then be used in clinical trials.
What are the ethical concerns about stem cell research?
Ethical concerns have been raised in the past about growing embryos solely for research purposes.
The UK has some of the most liberal laws concerning the manipulation of embryos for stem cells research and, as a result, is leading the way in this field, Donald Bruce, bioethics expert and managing director of the ethics consultancy Edinethics told Channel 4 News.
“It is controversial, but underlying that is the reluctant use of embryos, given there is such a benefit to be made.”
What medical conditions can be helped with stem-cell research?
A stem cell is a generic cell that can make exact copies of itself indefinitely, so it can produce specialised cells for any body tissues, and could potentially help treat a range of medical problems from blindness or diabetes to paralysis.
Have stem-cells been used to cure diseases?
The clinical use of ESCs is already being explored in very early stages in a number of safety trials to treat spinal cord injury and macular degeneration. However the cell lines used were reclassified from research grade to clinical grade through lengthy and expensive testing and validation.
In the early stages of stem cell research, people had huge expectations of its capacity for immediate use in therapeutic medicine. The actor Christopher Reeve famously moved to the UK because he thought stem cell therapy could cure him of Parkinson’s disease. But he died here in 2004.
Many pinned their hopes on the US biotech company, Geron, which tried to cure spinal injury chord in a trial using stem cell injections. While there were no ill-effects, the treatment also failed to improve any conditions and last month the company abandoned the trial, the first of its kind.
When will stem-cells be used to help with regenerative diseases?
There is still a long way to go, Professor Braude told Channel 4 News, adding that he had been asked this question since 2003: “This is a long-term strategy. They have to undergo further rigorous testing for all sorts of viruses and bacteria, grown up in larger batches and test that they stay normal.”
Any one line will take at least a year, says Professor Baude, but scientists are looking at 2014 before they can begin to consider the therapeutic impact.