NHS: nurses ‘no confidence’ in Health Secretary
Nurses deliver a vote of no confidence in Health Secretary Andrew Lansley as an emergency medicine consultant tells Channel 4 News about the shortages and pressures in NHS hospitals.

The Royal College of Nursing congress voted overwhelmingly in favour of a motion saying they have “no confidence” in Health Secretary Andrew Lansley over his management of wide-ranging NHS reforms.
It is the first time nurses have ever delivered a vote of no confidence in a Health Secretary. Delegates at the Liverpool conference voted 99 per cent in favour of the motion.
Angry delegates said Mr Lansley’s plans would ruin the NHS and lead to worse patient care. Nurse Geoff Earl said it was a “very, very serious issue.”
This is being driven by ideological dogma, not what is best for our patients. Nurse Geoff Earl
He said: “Mr Lansley says he wants to hear from us – well go out on the wards, go out into the community and listen to what our colleagues are saying.
“This is being driven by ideological dogma, not what is best for our patients.”
Bethann Siviter, from Birmingham, said if the reforms went ahead “the NHS is dying”.
Read more in the Channel 4 News Special Report: NHS uncovered
Mr Lansley is not giving a speech at the congress – causing some nurses to suggest he lacks “guts” – but will instead speak to a group of around 60 nurses later, in private, to try and allay their concerns over cuts and changes to the NHS. The outcome of the no confidence motion suggests he may have an uphill battle.
Lansley: ‘I am sorry’
The Health Secretary told a group of nurses at the conference: “If there is an ideology in what I am doing, it is a belief in the National Health Service.
“I want to enable the NHS to be stronger, and protect the NHS.”
Mr Lansley went on to apologise for failing to get the support from the delegates. He said: “I did read what was said this morning, and the result of the vote this morning, and from my point of view, therefore, I am sorry.”
“I am sorry if what it is I am attempting to do is not communicated.”
He told the gathered health professionals they all have “a shared objective”, which is for the NHS to be stronger, free, comprehensive, high quality and available to all based on need.
He told the nurses he wanted them, along with doctors and other health professionals, to have a central role in the delivery of care, and in the decision-making about care.
On hold
While the reforms are currently on hold as the Coalition Government consults further, the Royal College of Nursing is also extremely worried by spending and job cuts for the health service. On Monday, the RCN released figures suggesting that up to 40,000 jobs could go in the NHS – around half of which would be clinical posts.
After the vote, Mr Lansley said: “The nurses’ union support the principles of the Bill. But I know from listening to them that they want further nurse involvement in decisions. So do I.
“And I understand their concerns. We are listening to nurses and will make improvements. There isn’t an option to do nothing if we want to sustain the NHS for future generations.
“Any Government would be faced with the same challenges, only it would have been far worse under Labour because they wanted to cut the NHS budget, whereas we are investing an extra £11.5 billion into the service.”

Pressures
However, doctors are warning that the NHS already faces major pressures with limited resources – which more spending cuts would only exacerbate.
John Heyworth, President of the College of Emergency Medicine, told Channel 4 News: “The demand for emergency care is rising every year, between 4 and 7 per cent. We see almost 20 million patients a year in England.
“At the moment, we have an emergency care system which is not able to respond to that demand. A key element is staffing, which at the moment is woefully inadequate. We see almost 20 million patients but there are just 940 emergency medicine consultants.
“We would recommend 2,200 to allow more consultants to be in the hospital at weekends and evenings, when we get very sick patients in.”
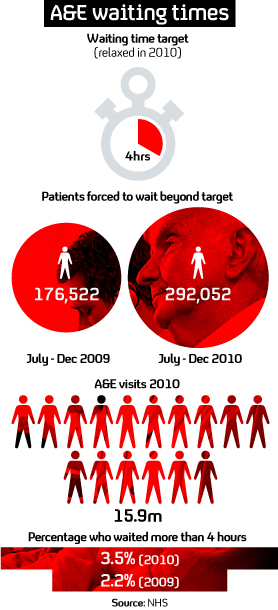
NHS figures show that waiting times have jumped 65 per cent since the Coalition Government scrapped waiting time targets. In June, Mr Lansley relaxed the four-hour waiting time target and the latest data shows that 292,052 people waited for more than four hours from July to December 2010. This compares to 176,522 people for the corresponding period in 2009.
At the moment, we have an emergency care system which is not able to respond to demand. Staffing is woefully inadequate. John Heyworth, President of the College of Emergency Medicine
Dr Heyworth told Channel 4 News that more consultants would save the NHS money at a time of austerity.
“We recognise the financial reality but appointing more consultants does save money,” he said. “We discharge more patients than less experienced doctors do, taking up less beds, and we order the right investigations, so saving money on expensive things like CT scans.”
He said it was very important that emergency medicine was taken into account by Mr Lansley as he looked at NHS reform – but said cuts would be very damaging.
“The public regards emergency care as one of the fundamental things the NHS delivers. At the moment we are not doing that, but the reforms provide us with the opportunity to get it right.
“We are very concerned about cuts. At the moment we have a system which is not coping with the current demand. We know demand will increase, so reducing emergency medicine staff is completely counterproductive.”
Shortage
One A&E consultant who spoke to Channel 4 News said that the pressure of a “24 hour society” as well as a lack of doctors was causing shortages in hospitals.
He said many hospitals were forced to operate with less than the College of Emergency Medicine‘s recommended eight to 10 consultants per department to operate safely. His own hospital only has five.
“There is a rising demand on emergency care. In some places annual attendances are rising by up to 10 per cent a year,” he said, speaking on condition of anonymity.
There’s a shortage of middle grade doctors – the workhorses of the NHS. A&E consultant
“There’s the old chestnut of difficult access to out-of-hours primary care, the ageing population – but part of it is the 24 hour culture we live in now. You can go shopping at 2 in the morning, why not see a doctor at 2 in the morning? Certainly 10 years ago from 10pm you only saw real emergencies whereas now throughout the day you see a variety. Sometimes things that could wait until the next day.”
He said the “middle grade tier” of doctors was missing in UK hospitals.
“Lots have gone overseas, to places like New Zealand and Australia, and discovered there’s a better way of life and a better way of working – so they ain’t coming back. So there’s a shortage of middle grade doctors – the workhorses of the NHS. Very few hospitals have that tier adequately filled. So everyone’s mucking in,” he said.
Waiting times
Last year, the Coalition Government changed the four hour waiting time target to make it less stringent, focusing instead on wider clinical aims. One A&E consultant told Channel 4 News that he hoped strongly that the change would not lead to a return to the "horrendous" waiting times of old.
"I hope as a group of emergency medicine consultants we focus on doing the best for patients so this remains at the forefront," he said.
"If you think what emergency medicine was like prior to the four hour target, there were people waiting for horrendously long times and in a way the service you were delivering just wasn't humanitarian. So the target made the service more patient focussed and was a bit of a revolution in emergency medicine.
"I hope most departments will continue to be sensible and pragmatic and see patients according to clinical need. The days of leaving patients sitting there for hours - I think they are gone and I am glad about that."